Sacrocolpopexy and sacral hysteropexy – Fact Sheets
What happens during surgery?
Are there any complications?
Recovery time
Vaginal prolapse is a common condition and can cause symptoms such as a sensation of a vaginal lump, constipation, and difficulty emptying the bowel or bladder or problems with sexual intercourse. An operation is only indicated when the prolapse is symptomatic. The majority of women will have improvement of symptoms following an operation.
Some women will be suitable to try a vaginal pessary instead of surgery. This is a device that supports the vagina and will be changed every 4 to 6 months.
Depending on the site of the prolapse, your doctor may suggest you have surgery that is performed from the abdomen. The vagina or uterus is then supported by mesh or stitches that are attached to the front of the tail bone (sacrum). This provides good support to the top of the vagina or uterus. A repair inside the vagina may also be required at the same time. The operation can be performed in combination with other procedures.
Studies from our hospital show that this operation is successful to support the top of the vagina or uterus in over 90% of women.
What happens during surgery?
The surgery is performed under general anaesthetic (you are completely asleep).
The operation may require an incision on your abdomen or be performed laparoscopically (key hole surgery). Your surgeon will advise you which method is best for you.
A subtotal Hysterectomy may be performed first if that was dictated. The uterine body and the tubes usually will be removed leaving the cervix attached in place. The ovaries may be removed at the same time if either indicated or requested prior to the surgery.
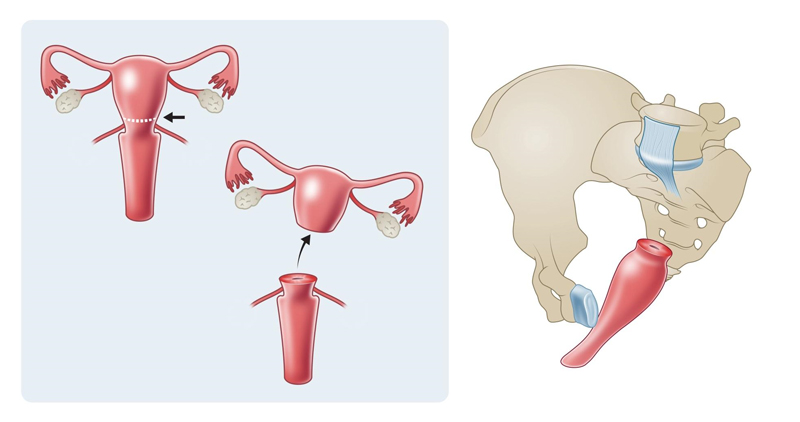
Figure1: Sub-total or partial hysterectomy It involves the removal of Fallopian tubes+/- the ovaries and the upper two-thirds of the uterus only, preserving the cervix.
The top of the vagina or the cervix is then stitched with permanent stitches or using mesh (a synthetic material) to the back of the tailbone (sacrum). This provides very strong support to the vagina or uterus.
The lining of the abdomen is then used to cover the stitches or mesh inside you.
A surgical repair of the vagina may be required, depending on the type of prolapse you have.
At the end of the operation, a catheter will be inserted into the bladder to drain urine and a material pack will be placed in the vagina to prevent bleeding. These will remain in place for 1-2 days.
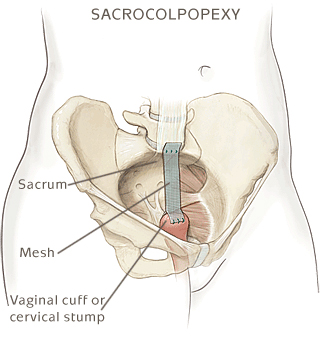
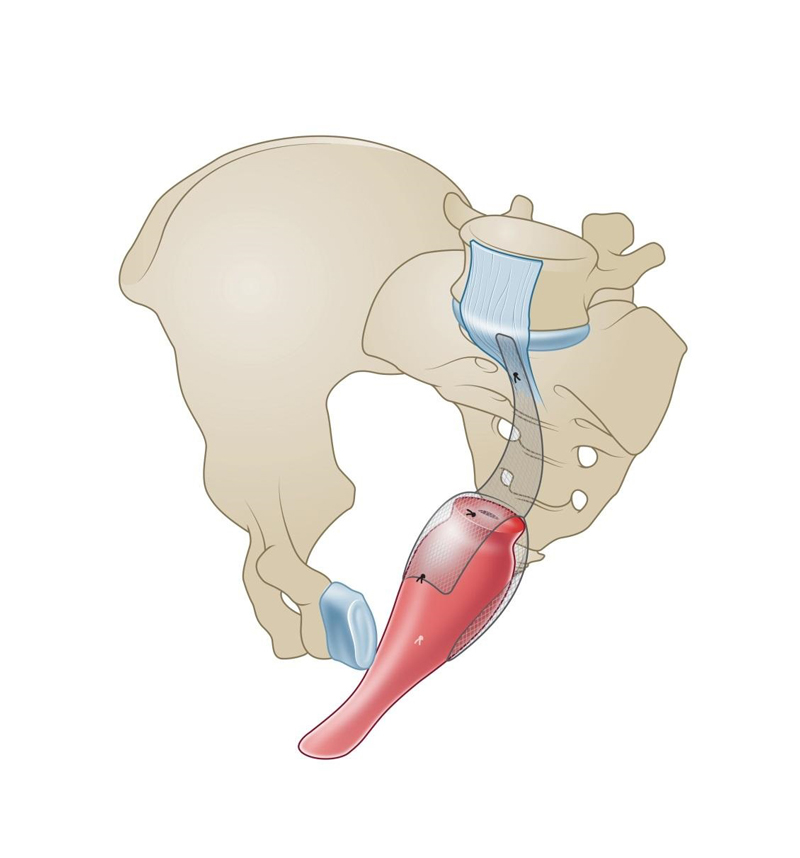
Figure2: Sacrocolpopexy and sacrocervicopexy (when the cervix is preserved) attaching the vagina to the level of sacral promontory.
Sacral Colpopexy:
This procedure is indicated in cases where the upper vagina (Vaginal Vault) is prolapsing generally with a history of having Hysterectomy in the past.
It is considered to be the Gold standard procedure to address such type of vaginal prolapse. It is achieved through having the vagina, including the front and the back wall suspended to the level of the sacral promontory.
The suspension is done through the use of a synthetic mesh sutured to the front and back wall of the vagina as well as to the vaginal “vault”. In turn the other end of the mesh is sutured to the ligament that is running in front of the backbone.
The procedure is done through keyhole surgery or Robotically.
Laparoscopic Sacral Hysteropexy:
This operation indicates that the uterus itself is prolapsing down through the vaginal canal. It entails having the uterus suspended and attached to the sacral promontory, the same location used to suspend the top of the vagina above. A strip of mesh is used and sutured to the back of the cervix while the other end of the mesh is sutured to “the tail bone”. Such procedure is offered for women requesting to preserve the uterus for fertility reasons or otherwise. It is important to realize that uterine preservation is not recommended when there is suspected uterine pathology or if the uterus is large and heavy.
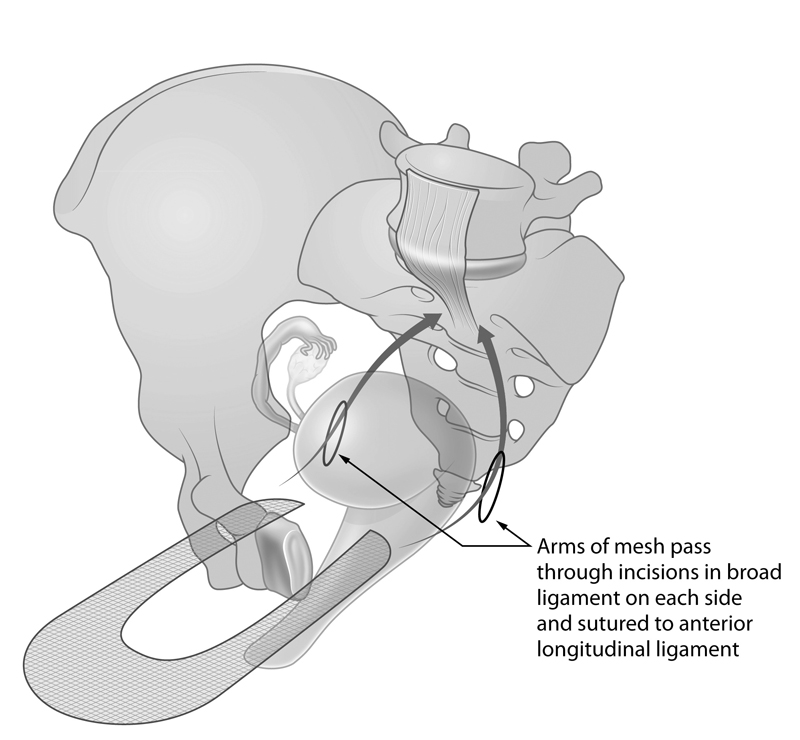
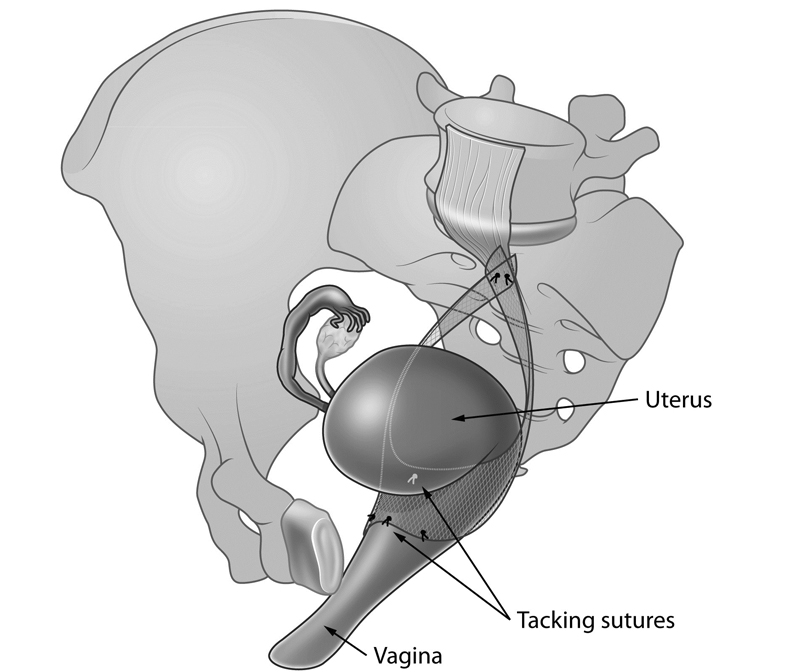

Figure3: Sacral Hysteropexy: Attaching the uterus to the level of the sacral Promontory.
Are there any complications?
If you are having keyhole surgery, there is a small possibility that this may need to be changed to a larger incision during the operation due to difficulties or to repair any unforeseen problems.
Possible complications and discomforts from surgery for prolapse include pain, infection, perforation of the rectum or bladder, and pain with intercourse.
Recurrence of symptoms and/or prolapse may occur. Usually this is in another site of the vagina, due to further weakness in the area.
If mesh is used, there is a small risk (about 2%) of mesh coming through the vagina. This is usually treated with oestrogen if the vaginal skin is thin or a small vaginal operation to cover the mesh.
The ureter (the tube running from the kidneys down to the bladder) could be damaged during the surgery. A cystoscopy (looking inside the bladder) will be performed at the end of the surgery to check that no damage has occurred.
There are general risks involved with having an operation, including the anaesthetic, bleeding and blood transfusion, infection within the pelvis or wound and clots in the legs that can travel to the lungs.
Recovery time
Most women stay in hospital for 4-5 days. You will be sent home once you are feeling well and once you are able to pass urine with no problem.
It is important to rest after the operation and allow the area to heal. Generally it is recommended:
- You restrict activity for two weeks.
- After 2 weeks do light activity only.
- Avoid heavy lifting for 6 weeks, including shopping bags, washing baskets and carrying children.
- Abstain from sexual activity for 6 weeks.
- Avoid playing sport for 6 weeks.
Please note Any surgical or invasive procedure carries risks. Before proceeding, you should seek a second opinion from an appropriately qualified health practitioner.
Disclaimer
Dr. Al-Salihi does not accept any liability to any person for the information (or use of such information), which is provided in this fact sheet or incorporated into it by reference. We provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy.