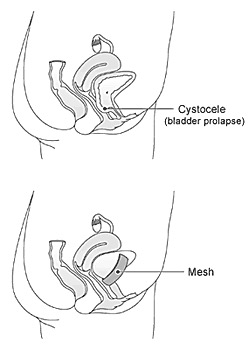
Vaginal Prolapse Surgery using tissue repair and using Mesh:
Vaginal prolapse is a common condition where the bladder, uterus and or bowel protrude into the vagina. This can cause symptoms such as a sensation of a vaginal lump, Dragging sensation and heaviness, constipation, and difficulty emptying the bowel or bladder or problems with sexual intercourse. Treatment is only indicated when the prolapse is symptomatic. The majority of women will have improvement of symptoms following an operation.
Surgery:
Depending on the severity of your symptoms and the type of prolapse your doctor may suggest you have surgery. The aim of surgery is to provide support for your vagina &/or uterus. Previous experience has shown that about 70% women undergoing conventional vaginal prolapse surgery have a successful outcome. Mesh reinforcement is used only with the aim of reducing the risk of recurrence of the prolapse. It may provide a longer lasting repair and has been shown to be successful in 80% of people. The use of surgical mesh to reinforce prolapse repair is not new.
Native tissue repair (No Mesh):
The procedure can be performed under regional or general anaesthesia.
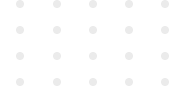
Anterior vaginal repair:
- Midline incision to the vagina overlying the bladder and urethra.
- Dissection in a plane directly below the vagina and lateral of the bladder allows the damaged fascia supporting the bladder to be exposed.
- The fascia (supporting tissue) is sutured together using desolving stiches.
Anterior vaginal fascial repair (using the native tissue to support the repairing compartment).
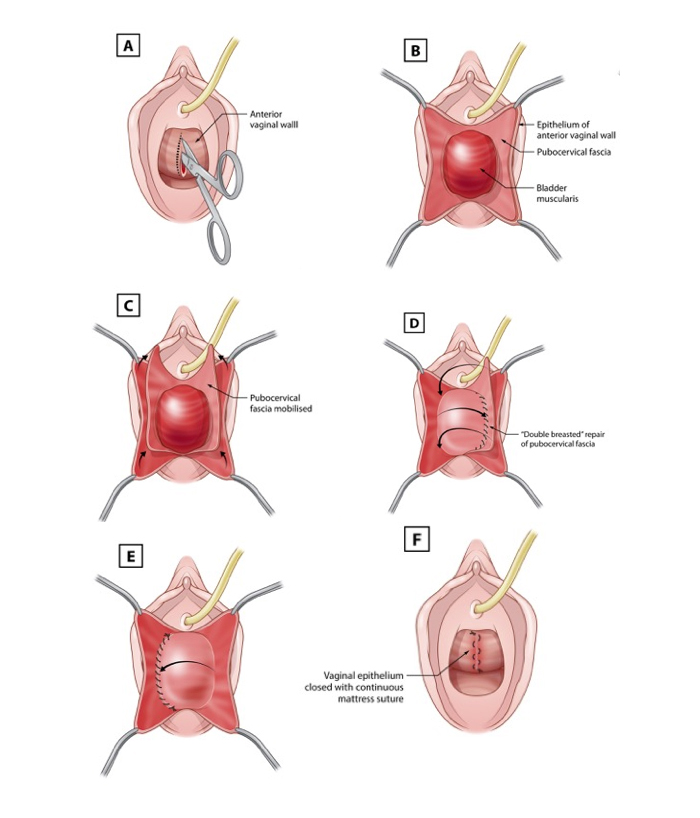
Posterior and vault repair:
- An incision is made to the posterior wall of the vagina.
- Dissection below the vagina identifies the fascia at the back and opens the space between the rectum and the pelvic floor muscle to the sacrospinous ligaments.
- Defects in the fascia are corrected by centrally placing sutures as described above.
Posterior vaginal wall repair (repairing the bowel side of the vaginal wall)
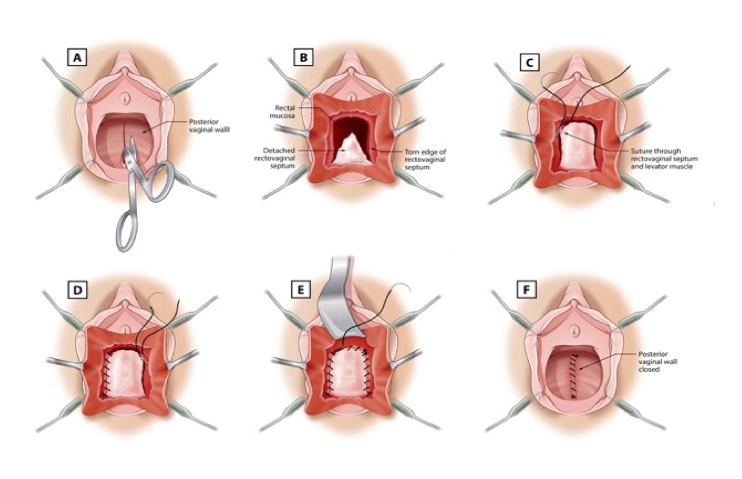
What is mesh?
Mesh is a synthetic material and is permanent.
Mesh has been extensively used in surgery, especially in hernia repairs.
The mesh has many holes within it to allow the bodies own tissue to grow into the mesh. The mesh then provides a framework of support.
Posterior vaginal repair (back wall)
Anterior Vaginal wall repair (front wall)
Success rate of the surgery is about 85 – 90%. Serious complications are rare with this type of surgery. However, no surgery is without risk and the main potential complications are listed below.
- 5-15% women will develop recurrent prolapse.
- Mesh erosion/infection 5-10%. Simple resuturing is usually sufficient but if infection persists further surgery may be required to remove the mesh.
- 1-5% develop a urinary tract infection.
- After a large prolapse is repaired urinary leakage may develop that was not present before the surgery 5%.
- Difficulties passing urine necessitating prolonged self-catheterisation postoperatively 1%.
- 1-5% constipation or failure to correct symptoms like incomplete bowel evacuation.
- Inadvertent damage to bladder, urethra, bowel or ureters occurs rarely and is usually repaired during surgery but further surgery may be required.
- Excessive bleeding requiring blood transfusion is uncommon (<1%).
- Clots can form in the legs or lungs after surgery
- Ongoing vaginal pain and/or persistent pain during intercourse (1-5%) that may require further surgery.
Recovery time:
Most women return home within 3 days of the operation. You will be sent home once you are feeling well and once you are able to pass urine with no problem. If you need pain relief, tablets are usually enough.
It is important to rest after the operation and allow the area to heal.
Generally, it is recommended that:
* You restrict activity for two –three weeks. In the early postoperative period you should avoid situations where excessive pressure is placed on the repair ie lifting, straining, coughing and constipation.
* After two-three weeks do light activity only
* Avoid heavy lifting for six weeks, including shopping bags, washing baskets and children.
* Abstain from sexual activity for six weeks.
* Avoid playing sport for four-six weeks.
Please note Any surgical or invasive procedure carries risks. Before proceeding, you should seek a second opinion from an appropriately qualified health practitioner.
Disclaimer
Dr. Al-Salihi does not accept any liability to any person for the information (or use of such information), which is provided in this fact sheet or incorporated into it by reference. We provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy.